What is ICD-10?
ICD-10 is the latest version of the International Classification of Diseases, a system of codes used to classify and report medical diagnoses and procedures. The transition from ICD-9 to ICD-10 brought significant changes to the healthcare industry, including the medical billing and coding process. In this blog post, we’ll discuss the impact of ICD-10 coding changes on medical billing.
More Specific Codes
ICD-10 includes a much larger number of codes than ICD-9, which allows for greater specificity in describing medical diagnoses and procedures. This increased specificity provides a more accurate reflection of the patient’s condition, which helps improve patient care and outcomes. However, it also means that medical coders must be more meticulous in their work to ensure that the correct codes are applied.
Increased Documentation Requirements
With the greater specificity of ICD-10 codes comes an increased need for detailed documentation. Medical coders require more information in order to accurately assign codes, which means that physicians and other healthcare providers must provide more thorough documentation. This can be time-consuming and challenging, particularly for smaller practices.
Training and Education Requirements
The transition from ICD-9 to ICD-10 required extensive training and education for medical coders and healthcare providers. The new coding system is much more complex than the previous version, and it requires a greater level of expertise to ensure accuracy. This training and education can be costly and time-consuming, particularly for smaller practices.
Delayed Reimbursements
One of the biggest concerns for medical practices during the transition to ICD-10 was the potential for delayed reimbursements. With the increased complexity of the new coding system, there was a risk that insurance companies and other payers would struggle to process claims in a timely manner. While there were some initial delays, the transition to ICD-10 has largely been successful, and most practices are now able to process claims in a timely manner.
Impact on Revenue Cycle Management
ICD-10 coding changes have also impacted revenue cycle management (RCM) for medical practices. With the increased specificity of codes, medical billing and coding teams must be more accurate in their coding and documentation to avoid claim denials and delays. This requires greater attention to detail and more thorough reviews of claims, which can slow down the RCM process. However, with proper training and education provided by Promed Billing Associates, your practice can optimize RCM processes to ensure timely reimbursements.
Quality Reporting
ICD-10 coding changes have also affected quality reporting for healthcare providers. Quality reporting measures are used to assess the quality of care provided by medical practices, and accurate coding is a key factor in these measures. The increased specificity of ICD-10 codes allows for more accurate quality reporting, which can lead to improved patient outcomes and better reimbursement rates for practices.
Impact on Data Analytics
ICD-10 coding changes have also had an impact on data analytics for medical practices. With the increased specificity of codes, practices can gather more detailed data on patient diagnoses and procedures. This data can be used to identify trends and patterns in patient care, which can lead to improved care delivery and better patient outcomes. ICD-10 coding changes has brought some challenges for medical practices, it has also provided opportunities for improvement in patient care, revenue cycle management, quality reporting, and data analytics. By staying up-to-date with coding changes and investing in training and education for their teams, practices can continue to thrive in the changing healthcare landscape.
2023 Coding Changes
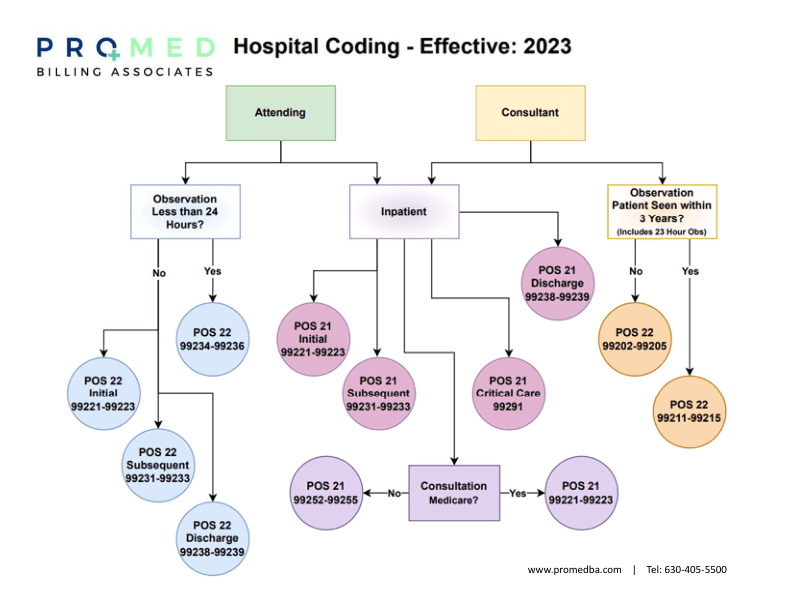
The Current Procedural Terminology (CPT) code set is used to report medical procedures and services performed by healthcare providers in the United States. Each year, the American Medical Association (AMA) releases updates to the CPT code set to reflect changes in medical practices and advances in technology. In this blog post, we’ll discuss the 2023 CPT hospital coding changes and their impact on healthcare providers.
New Codes for Remote Patient Monitoring
The 2023 CPT updates include several new codes for remote patient monitoring. These codes reflect the increasing use of technology in healthcare and the need to accurately report and bill for remote monitoring services. Remote patient monitoring involves the use of technology to monitor patient health outside of a traditional healthcare setting, such as in the patient’s home. The new codes allow for more accurate reporting and reimbursement for these services.
New Codes for Telehealth Services
The 2023 CPT updates also include new codes for telehealth services. Telehealth involves the use of technology to provide healthcare services remotely, and it has become increasingly popular in recent years. The new codes reflect the growing importance of telehealth services and allow for more accurate reporting and reimbursement.
Changes to Evaluation and Management Codes
The 2023 CPT updates include changes to the evaluation and management (E/M) codes, which are used to report office visits and other services provided by healthcare providers. The changes are intended to simplify the coding process and reduce documentation requirements. This will make it easier for providers to accurately report E/M services and reduce administrative burden.
New Codes for Genetic Testing
The 2023 CPT updates also include new codes for genetic testing. These codes reflect the growing importance of genetic testing in healthcare and the need to accurately report and bill for these services. The new codes will allow for more accurate reporting and reimbursement for genetic testing services.
Overall, the 2023 CPT updates reflect the ongoing changes and advancements in healthcare and the need to accurately report and bill for new and emerging services. Healthcare providers must stay up-to-date with these changes and ensure that their billing and coding practices reflect the latest updates to the CPT code set. By doing so, you can ensure accurate reporting and reimbursement, allowing more time to focus on what is most important: your patients! Contact Promed Billing Associates today for your free consultation and financial review.